New Rome IV Diagnostic Criteria for IBS
New criteria for diagnosing functional gastrointestinal (GI) disorders were released in June 2016. The Rome IV criteria reflect advances in basic science research and clinical trials since the Rome III criteria were published 10 years ago. This edition took 6 years to develop and involved input from 117 experts representing 23 countries.1 Rome IV has several important changes in how functional bowel disorders are described and diagnosed.
Rome IV criteria definitions
Functional GI disorders have a new definition. Rome IV defines them as follows: “Functional GI disorders are disorders of gut–brain interaction. It is a group of disorders classified by GI symptoms related to any combination of the following: motility disturbance, visceral hypersensitivity, altered mucosal and immune function, altered gut microbiota, and altered central nervous system processing.”1
All this to say that changes in many different body processes can lead to a functional GI disorder. In particular, a person may experience problems with:
- The movement of food and waste through the GI tract (“motility disturbance”)
- Heightened experience of pain in the internal organs (“visceral hypersensitivity”)
- Changes in the gut’s immune defenses (“altered mucosal and immune function”)
- Changes in the community of bacteria in the gut (“altered gut microbiota”)
- Changes in how the brain sends and receives from the gut (“altered central nervous system processing”)
Rome IV emphasizes that the best management for functional GI disorders requires a biopsychosocial approach.1 This approach takes into consideration:
- Early life influences: genetics, culture, environment.
- Psychosocial factors: stress, personality, psychological state, coping, social support.
- Physiology: motility, sensation, immune function, microflora, food, diet.
The stigma of IBS
Another important change is that the term “functional” has been removed wherever possible in Rome IV.1 The term does still appear, since there is no readily available substitute in some cases. However, the authors of Rome IV noted that the term “functional” is potentially stigmatizing and is not specific. Examples of this change include renaming “functional abdominal pain syndrome” as “centrally mediated abdominal pain syndrome,” and renaming “functional fecal incontinence” as “fecal incontinence.”
IBS diagnosis changes
The Rome criteria are important because they provide a standard definition of IBS. This is necessary for research and figuring out who can participate in a study.1 In actual practice, some people who do not exactly meet the criteria might still benefit from treatment. For them, the criteria are most useful for describing a particular condition.
Table 1 shows the Rome III and IV criteria side-by-side to highlight the changes.2,3
- Pain is still an essential part of the diagnosis, but the word “discomfort” has been removed. The authors believed that “discomfort” was vague and unclear. Another challenge is that not all languages have a word that means “discomfort,” which makes translation difficult.2
- The frequency of abdominal pain has increased slightly, from 3 days/month to 1 day/week.2 Before writing these updated criteria, the Rome Foundation conducted a survey to see how often people have gastrointestinal symptoms.1 The results were used to determine what is “normal.” The authors adjusted the criteria for some functional GI disorders, including IBS, based on the findings.
- The authors changed the phrase “improvement with defecation.” For many people, the pain does not improve with defecation. In fact, it may get worse.2
- The authors also removed the word “onset” from the other two criteria. As people with IBS know, the pain and change in stool frequency or form do not always coincide.2
| Rome III Criteria | Recurrent abdominal pain or discomfort at least 3 days/month in the last 3 months associated with two or more of the following:
aCriterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis. |
|---|---|
| Rome IV Criteria | Recurrent abdominal pain, on average, at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
cCriteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis. |
Source: Lacy BE, et al. Bowel Disorders. Gastroenterology. 2016;150:1393-1407; Rome III Diagnostic Criteria for Functional Gastrointestinal Disorders. Accessed 8/10/16 at: https://www.theromefoundation.org/
IBS subtypes
The three main subtypes of IBS are IBS-C (predominant constipation), IBS-D (predominant diarrhea), and IBS-M (IBS with mixed bowel habits), as shown below.2 People whose symptoms do not fit into any category are considered to have IBS unclassified.
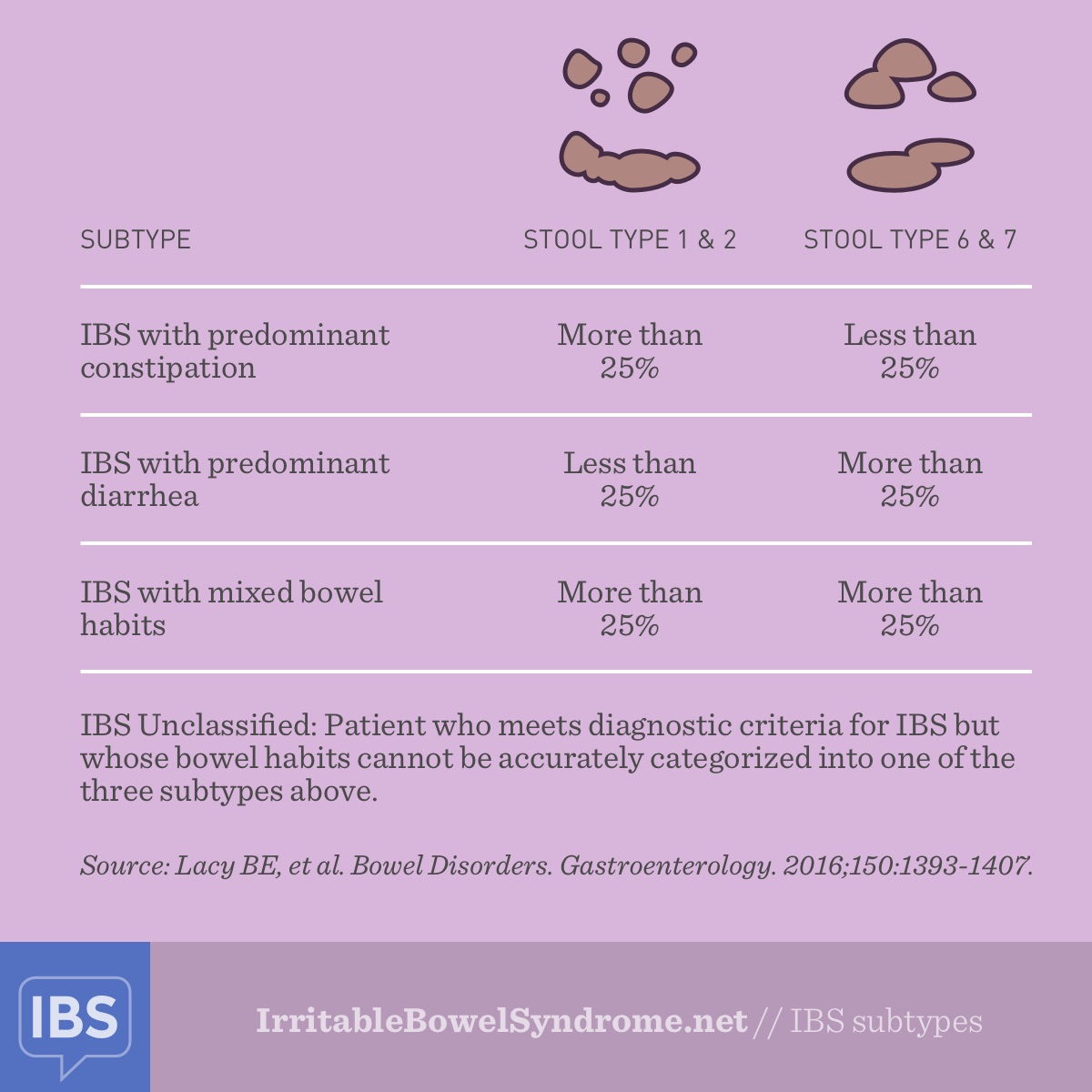
The subtypes have not changed, but Rome IV includes a slightly new way of identifying IBS subtypes. Subtypes are based on how frequently you experience very loose or very hard stools. The percentages are now based on stool form on days with at least one abnormal bowel movement.2 In Rome III, the percentages were based on total stools. Basically, the denominator has changed. This revision was made because some people have long periods of time with normal stool consistency. Your IBS subtype should be determined when you are not taking medications that treat bowel symptoms.
Rome IV clarifies that functional bowel disorders exist on a spectrum of symptoms.1 Furthermore, IBS subtypes are not separate conditions. The quantity, intensity, and severity of symptoms varies from patient to patient.1 The IBS subtype can be re-categorized as a person’s bowel habits change.
The rest of Rome IV
Rome IV is a comprehensive document that includes criteria for diagnosing all functional GI disorders. Several new diagnoses have been added, including:4
- Reflux hypersensitivity syndrome
- Cannabinoid hyperemesis syndrome
- Opioid-induced constipation
- Narcotic bowel syndrome
Rome IV includes a section called “Twelve Steps to Enhance the Therapeutic Relationship.”1 These steps provide physicians with guidance on partnering with patients to improve treatment and outcomes.
Several new chapters have been added, including one called “Intestinal Microenvironment and the Functional GI Disorders.”1 This chapter presents the latest research about the role of microbiome, food, and nutrition in GI function. The chapter on patient illness experience has been expanded, with more information about the role of age and gender in functional GI disorders.1

Join the conversation