Small Fiber Neuropathy: A Common Cause of IBS?
Last year, I came across an interesting article in Relief News, a media vertical sponsored through Harvard Medical School that focuses on issues related to chronic pain (disclaimer: I occasionally write for them, which is why I also keep up to date on their other articles). In particular, this article covered interesting new research out of Massachusetts General Hospital in Boston that indicated fibromyalgia and irritable bowel syndrome could both be either a result of or related to small fiber neuropathy – or more specifically, something dubbed "small fiber polyneuropathy," or SFPN.
What is small fiber neuropathy?
SFPN is a phenomenon where the small fiber nerves right below the surface of our skin become damaged – sometimes because our own immune systems are actually attacking them. When these small nerve fibers become damaged, it leads to interference in transmitting nerve signals properly and can therefore contribute to complications such as the widespread bodily pain one normally might associate with fibro or the gastrointestinal complaints common for IBS patients. In one of the studies, out of 41 patients with unexplained widespread first pain appearing before age 21, 98 percent had additional symptoms that also often included intestinal issues. Of all of these patients, skin biopsy results showed definitive diagnostic evidence of SFPN in well over half (59 percent) of them and probable SFPN in 17 percent.1
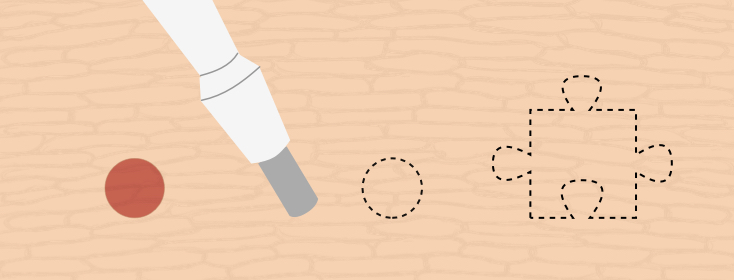
Intrigued by these findings, and living in the Boston metro area within relatively close proximity to Massachusetts General Hospital, I decided to have my own skin biopsied. The results were not all that surprising to me. Specifically, I scored an 11 percent for my biopsy, and those scoring under 15 percent are considered to be potential early or mild phase of SFPN, while those under 5 percent are considered definitively have full-blown SFPN (I am unsure what these percentages mean exactly but speaking to my neurologist about the results, it seemed to reflect the number of undamaged nerve fibers I have, which is low enough to cause nerve signal issues). While my score puts me in a grayer area, it definitely seems to offer another piece to the puzzle for my body's disruptions and complications, including those related to my gut.
IBS treatment
For the second phase of the study, patients were treated with either immunotherapy – or intravenous immunoglobulin (IVig) – 80 percent of whom experienced significant improvement. In another earlier study, several experienced relief from prednisone.2 The former treatment is pretty expensive and usually not covered by insurance. The second, while more widely available, is not without its risks side effects. However, I found it interesting because I noted that a few months after my laparoscopy for endometriosis, I was prescribed a week-long regimen of oral steroids for an unrelated disc rupture in my low back. I noted immediately after the regimen my IBS symptoms mostly disappeared for many months. They did eventually come back, and I am now intolerant to steroids, so that's not an option. But it's an interesting anecdote that seems to confirm these studies (at the time I honestly wondered if I was crazy for thinking the steroids could have helped my IBS).
For those for which this could be an option, getting a skin biopsy could help them uncover a possible cause or catalyst to their IBS and in doing so, consider treatments outside of the box or at least have the satisfaction of having the definitive results for a physical test to validate their experiences...which can go a long way in a society that still tends to be dismissive toward IBS.
Join the conversation